Understanding Acute Care Hospital Services DRG
Acute care hospital services DRG, or Diagnosis-Related Group, is a classification system used to categorize hospital stays into groups based on similar clinical characteristics and resource consumption. This system plays a crucial role in determining hospital reimbursement from Medicare and many private insurers. Understanding what acute care hospital services DRG entails is essential for both patients and healthcare providers. This knowledge empowers patients to navigate the complexities of the healthcare system and helps providers optimize resource allocation and ensure accurate billing. Read on to delve deeper into the intricacies of acute care hospital services DRG.
What Exactly Are Acute Care Hospital Services?
Acute care refers to short-term medical services provided to diagnose and treat illnesses or injuries that require immediate attention. These services are typically delivered in a hospital setting and address urgent medical needs. Common examples include emergency room visits, surgeries, and intensive care unit stays. The “acute” designation differentiates these services from long-term care, which focuses on ongoing management of chronic conditions. Acute care services are essential for addressing a wide range of medical issues, from broken bones to heart attacks. what drgs are acute care services
How DRGs Factor into Acute Care Hospital Services
DRGs categorize patients based on their diagnoses, procedures, age, and other factors. Each DRG is assigned a specific weight reflecting the average resources required to treat patients within that group. This weight is then used to calculate the reimbursement amount the hospital receives. The DRG system incentivizes hospitals to provide efficient and cost-effective care, as they receive a fixed payment regardless of the actual resources used for a specific patient.
Why are Acute Care Hospital Services DRGs Important?
Acute care hospital services DRGs are crucial for several reasons:
- Cost Control: DRGs help control healthcare costs by providing a standardized payment system.
- Efficiency: They encourage hospitals to provide care efficiently by rewarding those that deliver quality care within the allocated budget.
- Data Analysis: DRGs provide valuable data for analyzing healthcare trends and resource utilization.
- Transparency: The system offers a level of transparency in hospital billing practices.
Decoding the DRG System
Understanding the DRG system can seem complex. However, breaking it down into key components can make it more manageable:
- Diagnosis: The primary diagnosis driving the hospital stay is the most significant factor in determining the DRG.
- Procedures: Any procedures performed during the hospital stay are also considered in DRG assignment.
- Comorbidities and Complications (CCs and MCCs): Secondary diagnoses that impact the complexity of care, referred to as CCs and MCCs, also influence the DRG.
- Age and Discharge Status: Patient age and discharge status (e.g., home, rehabilitation facility) further refine the DRG assignment.
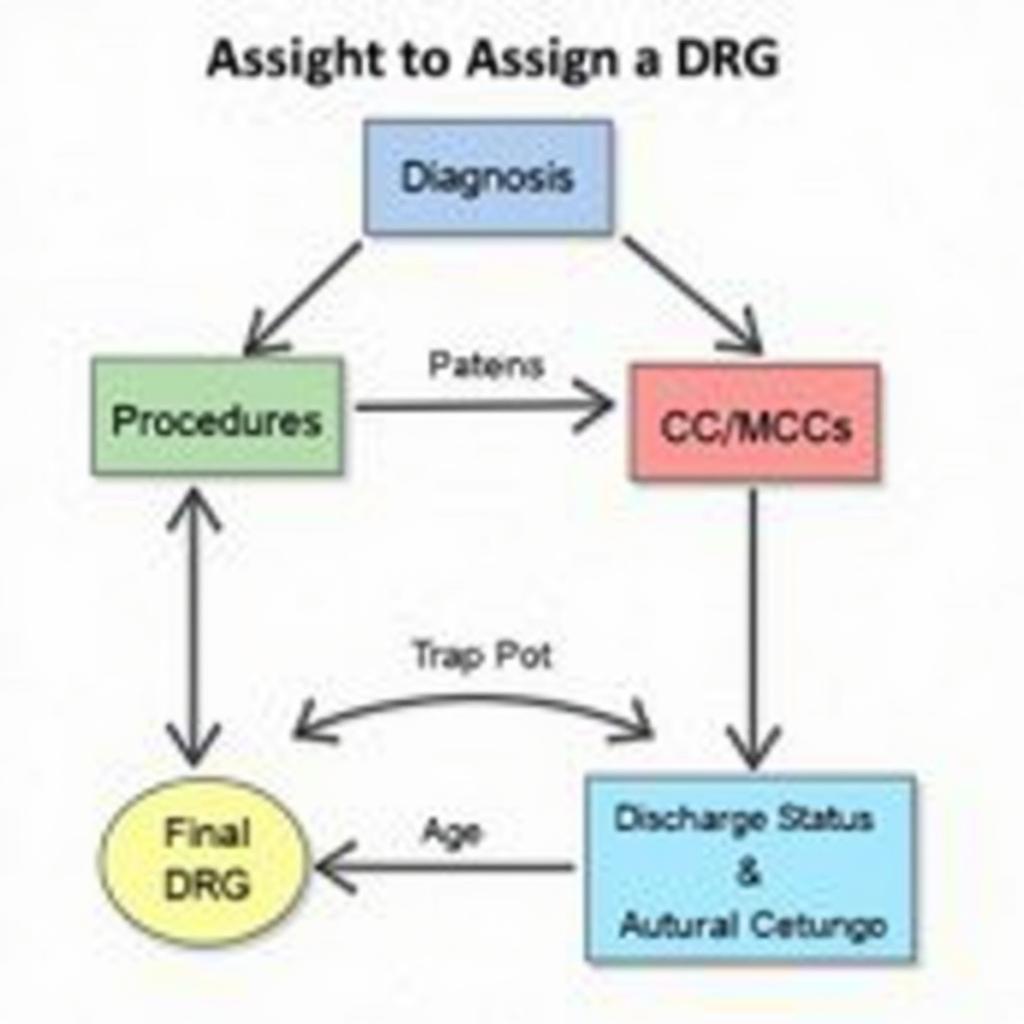 Diagram of the Acute Care Hospital DRG Coding System
Diagram of the Acute Care Hospital DRG Coding System
What Does This Mean for Patients?
For patients, understanding acute care hospital services DRGs can help them:
- Estimate Costs: While not always precise, DRG information can provide a general idea of potential hospital charges.
- Understand Billing: Patients can use DRG information to clarify their hospital bills and ensure accuracy.
- Advocate for Their Care: Knowing the DRG system can empower patients to ask informed questions and advocate for appropriate care.
“Understanding the DRG system empowers patients to be active participants in their healthcare journey,” says Dr. Amelia Carter, a leading healthcare economist.
What Does This Mean for Healthcare Providers?
For healthcare providers, DRGs are crucial for:
- Revenue Cycle Management: Accurate DRG coding is essential for proper hospital reimbursement.
- Resource Allocation: DRGs inform resource allocation decisions, ensuring efficient use of hospital resources.
- Quality Improvement: DRG data can be used to identify areas for quality improvement and cost reduction.
“Efficient DRG management is paramount to the financial health of any hospital,” adds Dr. Michael Reed, a seasoned hospital administrator.
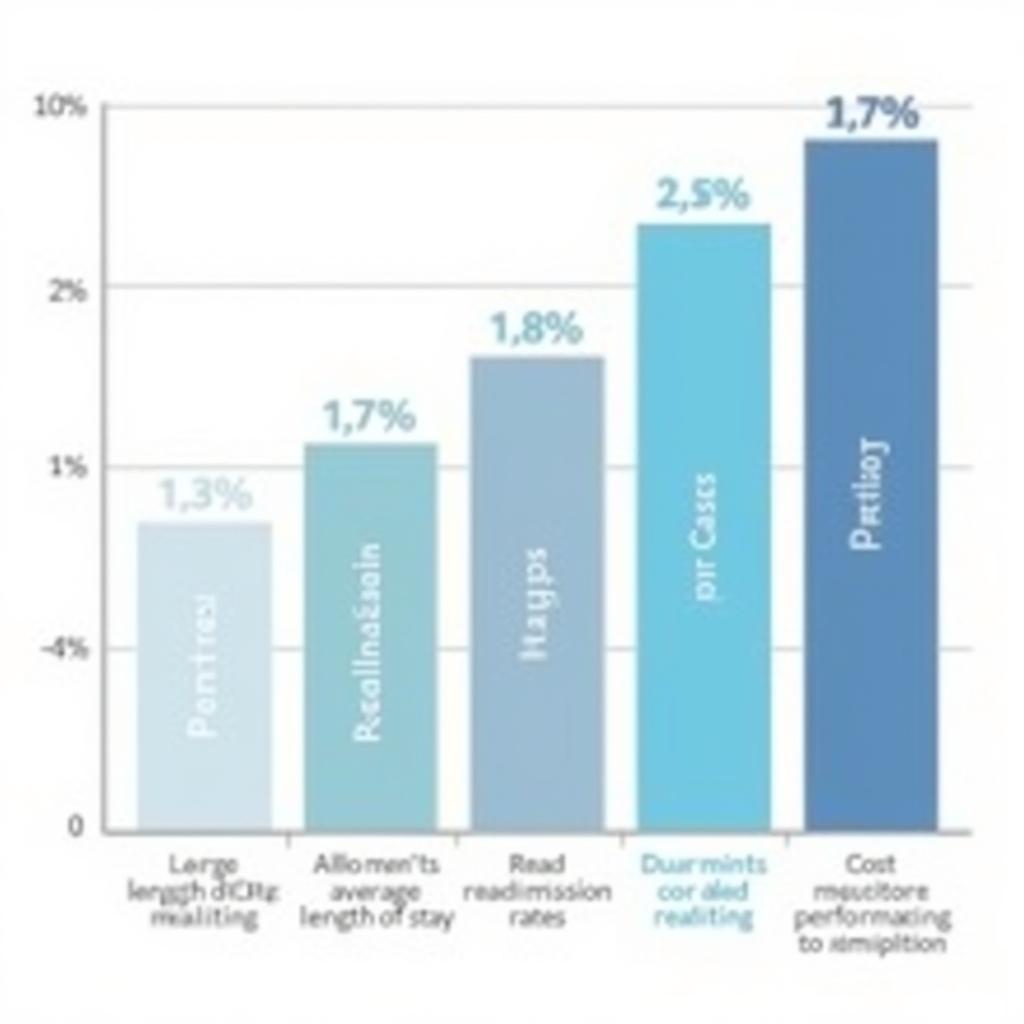 Graph Showing the Impact of Acute Care Hospital DRGs on Healthcare Providers
Graph Showing the Impact of Acute Care Hospital DRGs on Healthcare Providers
what is respiratory care services
Conclusion
Acute care hospital services DRG is a complex but essential part of the healthcare system. Understanding its implications can empower patients and help healthcare providers deliver efficient and cost-effective care. By grasping the fundamentals of acute care hospital services DRG, individuals can better navigate the healthcare landscape and make informed decisions regarding their care.
FAQ
- What does DRG stand for? DRG stands for Diagnosis-Related Group.
- How are DRGs determined? DRGs are determined based on diagnosis, procedures, age, and other patient characteristics.
- Who uses DRGs? Medicare and many private insurers use DRGs to determine hospital reimbursement.
- How do DRGs impact hospital billing? DRGs determine the fixed payment amount hospitals receive for each patient stay.
- Can patients access their DRG information? Yes, patients can typically find their DRG information on their hospital bill.
- Do DRGs apply to all hospital stays? While most inpatient stays are categorized under DRGs, certain exceptions may apply.
- How can I learn more about my specific DRG? Consult with your healthcare provider or hospital billing department for more detailed information.
Need further assistance? Contact us via WhatsApp: +1(641)206-8880, Email: [email protected] or visit our office at 456 Oak Avenue, Miami, FL 33101, USA. Our customer service team is available 24/7.