What Are Managed Care Services?
Managed care services coordinate patient care to control costs and improve quality. They work by negotiating discounted rates with healthcare providers, requiring pre-authorizations for certain procedures, and emphasizing preventive care. This approach aims to provide comprehensive healthcare while managing expenses effectively. After this brief overview, let’s delve deeper into managed care services. For those curious about how managed care might affect their chronic care needs, this article will also discuss the impact of managed care on chronic care services.
Managed care plans operate on a system of networks, connecting patients with healthcare providers contracted with the plan. These networks include primary care physicians, specialists, hospitals, and other healthcare facilities. Members typically need to choose a primary care physician (PCP) within the network, who acts as the gatekeeper for referrals to specialists or other services. This coordinated approach aims to streamline care and ensure appropriate utilization of resources. Who receive managed health care plan services, you might ask? A wide range of individuals and families across various demographics utilize these plans. It’s an increasingly common way to access healthcare. One of the key benefits of managed care is the emphasis on preventive care, which includes regular check-ups, vaccinations, and screenings. By focusing on early detection and disease management, managed care aims to improve overall health outcomes and reduce the need for expensive treatments in the long run.
Understanding the Core Components of Managed Care
Managed care involves a complex interplay between various stakeholders, including patients, healthcare providers, insurers, and employers. The core objective is to deliver high-quality care efficiently and cost-effectively. This is achieved through several key mechanisms:
- Network Management: Managed care organizations (MCOs) contract with a select group of healthcare providers to create a network. Members are generally required to receive care within this network to enjoy the full benefits of their plan. Going out-of-network usually means higher out-of-pocket costs.
- Utilization Management: This involves strategies to control the use of healthcare resources. Pre-authorization for certain procedures, second opinions for surgeries, and case management for chronic conditions are examples of utilization management techniques.
- Quality Management: MCOs have programs in place to ensure the quality of care provided within their network. These programs may involve credentialing providers, reviewing treatment outcomes, and implementing quality improvement initiatives. You might wonder, how do managed care organizations ensure quality services? They utilize a variety of methods, from regular audits to patient satisfaction surveys.
- Cost Containment: By negotiating discounted rates with providers, promoting preventive care, and managing utilization, managed care plans strive to control healthcare costs for both members and employers.
 Managed Care Network Illustration
Managed Care Network Illustration
Different Types of Managed Care Plans
Several different types of managed care plans exist, each with its own structure and level of flexibility:
- Health Maintenance Organizations (HMOs): HMOs generally require members to choose a primary care physician (PCP) who acts as a gatekeeper for all other healthcare services. Referrals from the PCP are typically needed to see specialists or receive other specialized care.
- Preferred Provider Organizations (PPOs): PPOs offer more flexibility than HMOs. While members can choose any provider, they receive greater benefits when using providers within the PPO network. Referrals are usually not required to see specialists.
- Point of Service (POS) Plans: POS plans combine features of both HMOs and PPOs. Members usually choose a PCP, but they have the option to see out-of-network providers, though at a higher cost.
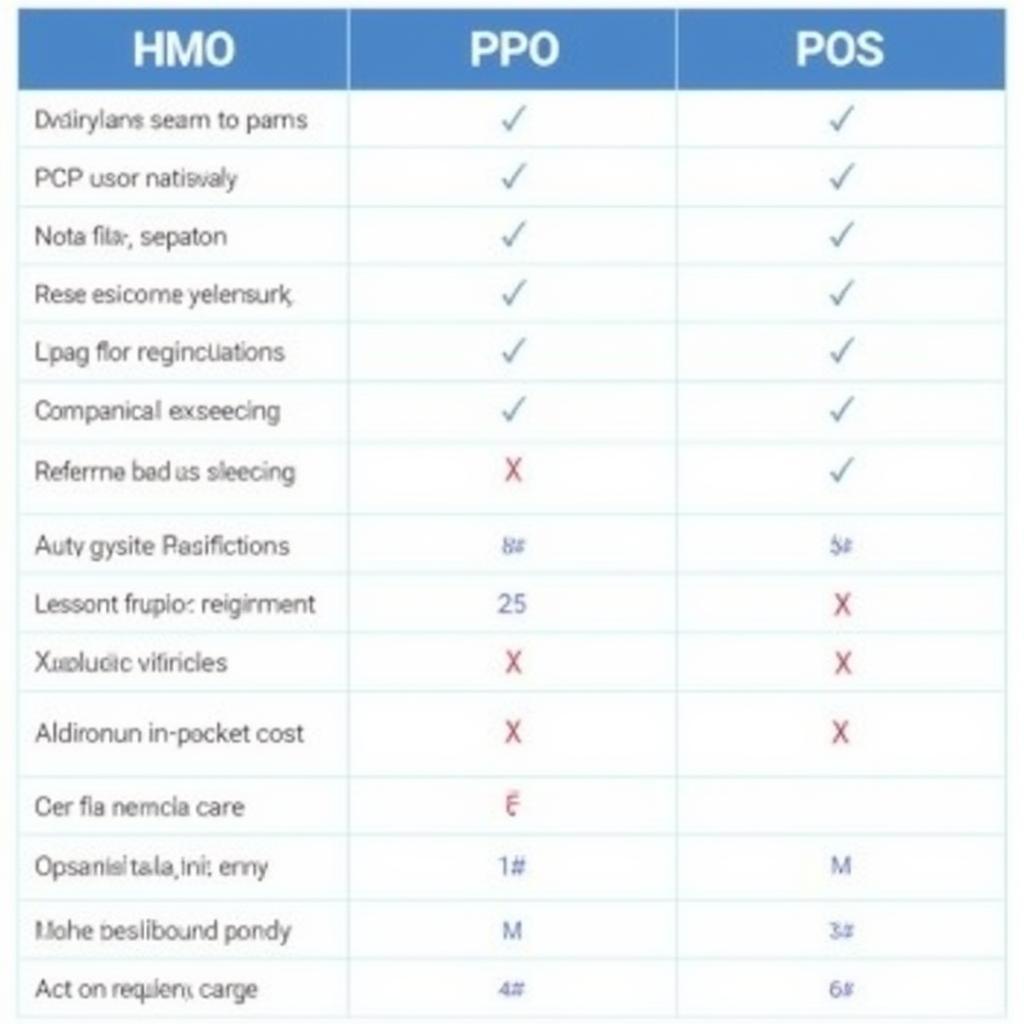 Types of Managed Care Plans Comparison
Types of Managed Care Plans Comparison
The Impact of Managed Care on Chronic Care
The shift towards managed care has significant implications for individuals with chronic conditions. Does managed care limit services for chronic care? Not necessarily. Managed care programs often implement specific strategies to address the needs of individuals with chronic illnesses, such as disease management programs and case management services. These programs aim to coordinate care, improve adherence to treatment plans, and enhance overall health outcomes. One specific example of a managed care service provider is A-1 Managed Care Services LLC. As Medicaid programs increasingly adopt managed care models, it’s important to understand the implications. Do services change when Medicaid adopts managed care? This can vary depending on the specific program and state, but the overall goal remains to provide cost-effective and coordinated care.
Conclusion
Managed care services aim to improve the efficiency and effectiveness of healthcare delivery while managing costs. By coordinating care, emphasizing preventive services, and implementing utilization management strategies, managed care strives to provide high-quality, affordable healthcare. Understanding the different types of managed care plans and their impact on chronic care is essential for navigating the complex healthcare landscape.
FAQ
- What is the main difference between an HMO and a PPO?
- How does managed care affect my choice of doctors?
- What are the benefits of preventive care?
- How can I find a managed care plan that meets my needs?
- What is the role of a primary care physician in managed care?
- What is utilization management, and how does it work?
- How can I appeal a denial of coverage under managed care?
Need support? Contact us via WhatsApp: +1(641)206-8880, or Email: [email protected]. Our customer service team is available 24/7.

