Are Telehealth Services Covered for Medicaid Schizophrenia Care?
Telehealth has revolutionized healthcare access, especially for individuals with serious mental illnesses like schizophrenia. Many are asking, Are Telehealth Services Covered For Medicaid Schizophrenia Care? This article delves into Medicaid coverage for telehealth services specifically for schizophrenia, exploring the benefits, limitations, and future of this innovative approach to mental healthcare.
Understanding Medicaid Coverage for Telehealth and Schizophrenia
Medicaid, a joint federal and state program, provides healthcare coverage to millions of low-income Americans, including many individuals with schizophrenia. The coverage of telehealth services for schizophrenia under Medicaid can vary significantly by state. While the federal government sets baseline requirements, states have flexibility in determining the specific services covered, reimbursement rates, and eligible providers. This variability stems from differing state regulations, available resources, and the unique needs of their populations. are telehealth services covered for medicaid schizoprenia care helps navigate these nuances and offers valuable insights.
Navigating State-Specific Medicaid Telehealth Policies for Schizophrenia
Because Medicaid telehealth coverage for schizophrenia isn’t uniform across all states, it’s crucial to research your state’s specific policies. Some states may cover a wide range of telehealth services, including individual therapy, medication management, and even group therapy sessions, while others may have more restrictive coverage. Understanding these differences is essential for both patients and providers to ensure access to necessary care. This can sometimes involve contacting your state’s Medicaid office directly or consulting resources provided by mental health advocacy organizations.
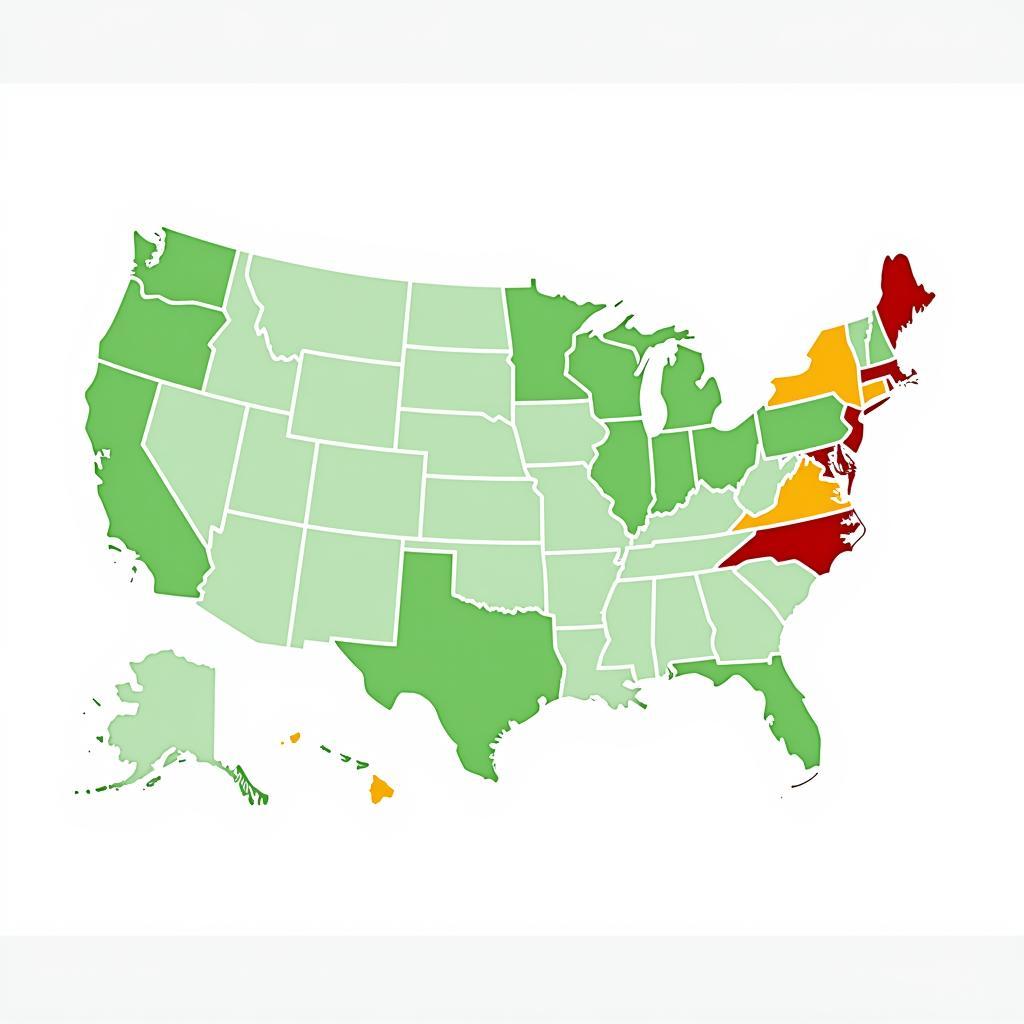 Medicaid Telehealth Coverage Map by State
Medicaid Telehealth Coverage Map by State
Benefits of Telehealth for Schizophrenia Care
Telehealth offers numerous benefits for individuals with schizophrenia, including increased access to care, particularly for those in rural areas or with limited mobility. It can also reduce stigma associated with seeking mental health treatment and provide a more comfortable and convenient setting for some individuals. The ability to connect with providers remotely can significantly improve treatment adherence and outcomes.
Does Medicaid Cover all Types of Telehealth for Schizophrenia?
While many states cover a range of telehealth services for schizophrenia under Medicaid, the specifics can vary. Not all types of telehealth may be covered, and there might be restrictions on the frequency or duration of sessions. For instance, some states may prioritize covering individual therapy via video conferencing but have limitations on coverage for remote medication management or group therapy sessions. It’s important to understand these nuances to effectively navigate the system.
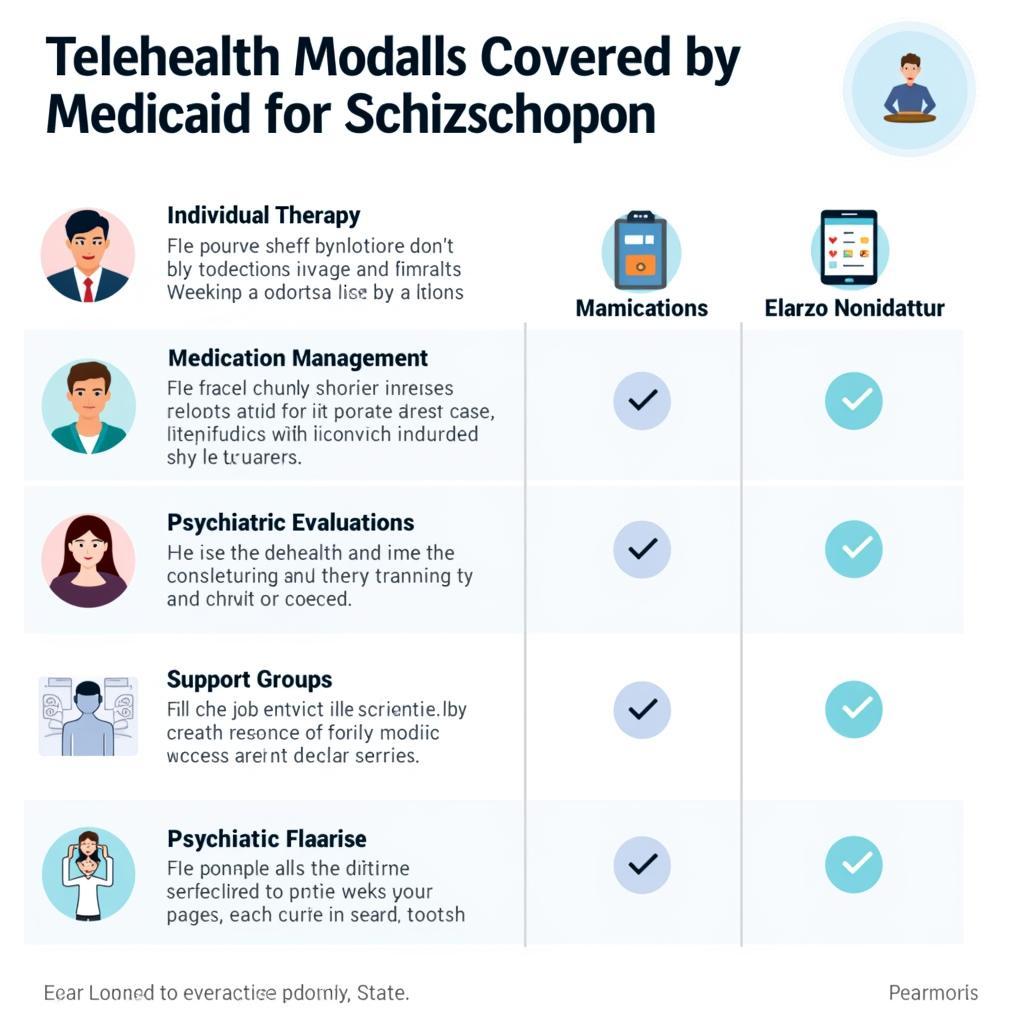 Types of Telehealth Services Covered by Medicaid for Schizophrenia
Types of Telehealth Services Covered by Medicaid for Schizophrenia
How to Access Medicaid Telehealth Services for Schizophrenia
Accessing telehealth services for schizophrenia under Medicaid usually begins with contacting your state’s Medicaid office or your health plan. They can provide information about covered services, eligible providers, and the process for accessing care. Many mental health providers now offer telehealth options, so it’s also helpful to inquire directly with potential providers about their telehealth services and how they bill Medicaid. which managed long term care program covers mental health services offers further insights into managing long-term care for mental health.
The Future of Medicaid and Telehealth for Schizophrenia
The landscape of telehealth is constantly evolving, and Medicaid policies are adapting to reflect the increasing role of technology in healthcare. The expansion of telehealth services for schizophrenia is a promising trend, with the potential to significantly improve access to quality mental healthcare. Ongoing advocacy and policy changes are crucial to ensure that individuals with schizophrenia can benefit from the advancements in telehealth technology.
 Future Trends in Telehealth and Medicaid for Schizophrenia Care
Future Trends in Telehealth and Medicaid for Schizophrenia Care
Conclusion
Accessing quality mental healthcare is essential for individuals with schizophrenia, and telehealth offers a valuable pathway to care, especially through Medicaid. While coverage varies by state, understanding the specifics of your state’s Medicaid telehealth policies is crucial. By staying informed and advocating for expanded access, we can leverage the power of telehealth to improve the lives of those living with schizophrenia. Are telehealth services covered for Medicaid schizophrenia care in your state? Research and find out – it could make all the difference.
FAQs
- What are the common telehealth services covered for schizophrenia under Medicaid?
- How do I find a telehealth provider who accepts Medicaid?
- What if my state’s Medicaid doesn’t cover the telehealth services I need?
- Are there any out-of-pocket costs for telehealth services under Medicaid?
- How do I ensure the confidentiality of my telehealth sessions?
- What equipment do I need for telehealth sessions?
- Can I use telehealth for medication management?
Need support? Contact us via WhatsApp: +1(641)206-8880, Email: [email protected], or visit our office at 456 Oak Avenue, Miami, FL 33101, USA. Our customer service team is available 24/7.